Evolution of Nursing: History, Advancements, and Accomplishments

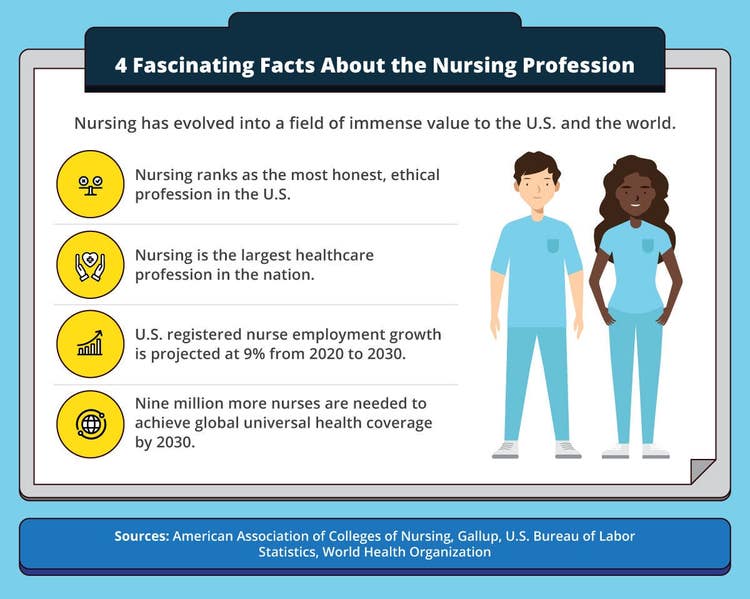
If trustworthiness were the ultimate prize in an annual sports event in which different career fields competed against each other, the nursing profession would hold one of the longest streaks in the history of that sport. Consider that for 20 consecutive years, the nursing profession has had the highest ethics ranking among professions, according to a Gallup poll. While the healthcare industry as a whole saw a slight decrease in public perception in 2021 amid the COVID-19 pandemic, the nursing profession held its ground as the most trusted profession.
The evolution of nursing, and its positive image, was sparked in the 19th century with Florence Nightingale. Her contribution to contemporary nursing began in 1854 when she led a corps of nurses to tend to sick and fallen British soldiers during the Crimean War. Since then, the nursing profession has evolved and has played an essential role in transforming society.
In investigating the evolution of nursing, seeing how nursing has changed over time and discussing key figures in the history of nursing are essential. Additionally, looking at developments in nursing and identifying trends can help provide a glimpse into the future of nursing.
Evolution of Nursing Overview
Modern-day nursing is very different from the time of the Crimean War and different from the time of both World Wars. Nursing was considered more of a helping role than a professional career.
Today, nurses have a broader range of practice options. They can work in various specializations and focus areas, such as ambulatory care, cardiac care, and emergency rooms, or as certified nurse-midwives (CNMs) or family nurse practitioners (FNPs). Nurses also have various responsibilities, from educating patients on self-care practices to prescribing and administering medications.
The evolution of nursing from a smaller-scope profession to a field with many specialties is primarily a result of improved nursing practice education. Each nursing area requires different skills, so no matter where nurses are in their careers, they can opt to advance their education to expand their skill sets and practice knowledge.
History of Nursing
Historical documents point to the origin of professional nursing at around A.D. 300, during the Roman Empire. But the evolution of nursing into a modern profession occurred centuries later amid a war-torn Europe. These are key highlights in the history of nursing:
- Following the collapse of the Roman Empire in A.D. 476, the eastern part of the empire survived, becoming the Byzantine Empire. Here, nursing began rising to For example, in Constantinople during this time, two hospitals were built that had male and female nurses.
- The history of nursing continued from the Middle Ages in Europe to the 10th and 11th centuries. During this time, nurses began working as part of monasteries and other religious organizations.
- The roots of modern nursing began forming in the 18th and 19th centuries. In North America and Britain, health services were expanded and categorized into different nursing branches — the origin of nursing specialties. However, no uniform set of nursing practices existed across these geographic areas.
- When the Crimean War began, nursing advanced into a profession that more closely resembles today’s nursing practice, compared with earlier forms of nursing. The war heightened the need to treat infection-related illnesses and battle wounds that required amputation or suturing, and nurses whom Nightingale led stepped up to provide care on the front lines of the war.
Women in Nursing
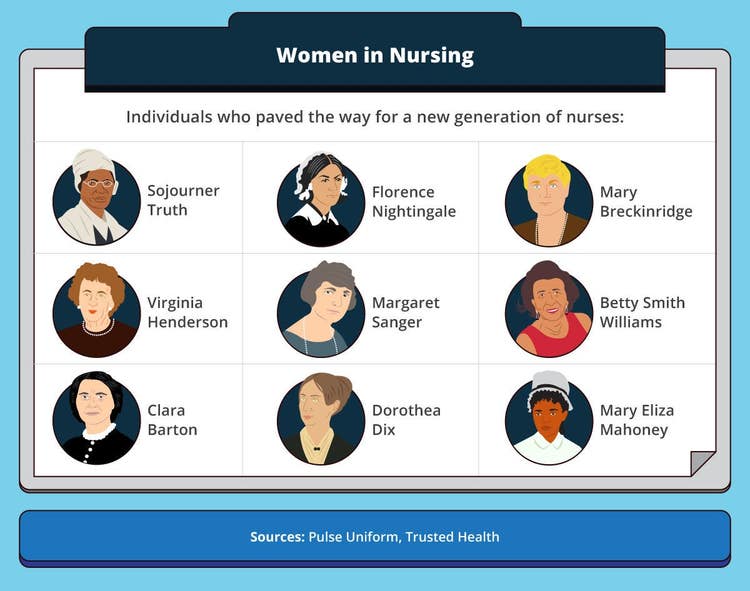
Women such as Nightingale, traditionally recognized as the founder of modern nursing, greatly influenced nursing. Following her leadership role during the Crimean War, Nightingale would open the first nursing school in London in 1860.
Over the centuries, many women have contributed to the evolution of nursing. One of the hidden figures of nursing history is famed abolitionist Sojourner Truth. She went from being a live-in nurse as a slave for the Dumont family to an appointee at Freedman’s Hospital, providing nursing care for patients. Throughout her life, Truth advocated for nursing education.
The history of women in nursing includes contributions from the following historical figures:
- Mary Breckinridge. As a nurse in World War I, Mary Breckinridge believed that nursing and midwifery could help bring much-needed healthcare to rural America. She founded and launched a service that included nurses on horseback to serve people in rural Kentucky. The service, which was later named the Frontier Nursing Service in 1928, reached more than 1,000 families in rural areas over 700 square miles.
- Virginia Henderson. Virginia Henderson has helped advance nursing science, from her teaching career launched in 1923 at Norfolk Protestant Hospital, through the extensive research she conducted at Yale University School of Nursing until 1996. Her contributions include authoring several editions of the Textbook of the Principles and Practice of Nursing and the need theory, which focuses on helping educate and encourage patients to become more independent in their care.
- Margaret Sanger. Among history’s most famous nurses is Margaret Sanger. She’s also considered one of the most controversial figures, advocating for birth control when the practice was deemed radical and obscene. Facing the threat of prosecution, she fled to England, where she continued to promote birth control through her writings. Upon returning to the U.S., she advocated for birth control amid prosecution and arrests. Her contributions led to the founding of the International Planned Parenthood Federation (IPPF) in 1952, and ultimately, the Supreme Court’s decision to legalize birth control in 1965.
- Betty Smith Williams. Minority rights activist, nurse, and administrator Betty Smith Williams was the first Black nursing school graduate from Case Western Reserve University. Later in her career, she broke even more barriers as the first Black person to teach at a California college or university. Her contributions to promoting opportunities for Black nurses included cofounding the National Black Nurses Association (NBNA). The American Academy of Nursing welcomed Williams as a fellow in 1980.
- Mary Eliza Mahoney. For 15 years, Mary Eliza Mahoney worked at the New England Hospital for Women and Children in various roles, including maid, cook, and nurse’s assistant. In 1879, she became the first Black woman to receive professional training and graduate from nursing school. Mahoney, recognized as the first Black nurse, became a member of the Nurses Associated Alumnae of the United States and Canada in 1896, which later became the American Nurses Association (ANA). Due to the organization’s primary focus on white nurses and delay in accepting women of color, Mahoney helped found the National Association of Colored Graduate Nurses (NACGN).
Women Nursing in the Civil War
During the American Civil War, the evolution of nursing continued. For example, before the war, women typically provided care to sick family members privately. In the first few months of the war, it became clear that women were needed to support the war effort. Male nurses on the battlefield were soldiers themselves, and as a result, many became casualties of the conflict, limiting nursing resources.
An estimated 620,000 soldiers died during the Civil War, many due to wound-related disease and infection. Soldiers needed care for the wounds, and women volunteered. During the war, women took more prominent public nursing roles, creating opportunities and inspiration for women in nursing careers after the war.
Women in nursing in the Civil War influenced the beginning of nursing as a profession after the war, including establishing standards of care and schools to promote nursing as a career further. Two prominent figures who advanced nursing during this time were:
- Dorothea Dix. In addition to serving as superintendent of Army nurses during the Civil War, overseeing Union Army nurses, Dorothea Dix was an activist who set guidelines to protect women in nursing, a field that men dominated. She also advocated for mental health and poor people throughout her career, lobbying to improve mental health hospital and prison conditions.
- Clara Barton. Clara Barton is famous for being the founder of the American Red Cross. She was inspired to start the organization in the U.S. after traveling and volunteering in Europe, where she learned firsthand about the International Committee of the Red Cross. Earlier in her career, she was a nurse on the Civil War battlefield, earning the name Angel of the Battlefield.
How Has Nursing Changed Over Time?
Nursing has changed over time, especially in the areas of nursing practice and education. For example, nurses have a broad range of choices for practice options and specializations. A nurse can choose a nurse practitioner (NP) track and acquire the clinical knowledge and essential skills to perform similar activities as doctors, including prescribing medicines in states with full practice authority. Common activities that nurses perform in their jobs include the following:
- Taking vital signs
- Drawing blood samples
- Recording medical histories on electronic health records (EHRs)
- Assessing and determining symptoms
- Conducting physical examinations
- Ordering or conducting diagnostic tests
- Working with physicians to recommend care options
- Providing education on self-care
- Administering medication
Nurse responsibilities have expanded over time with the heightened importance of patient safety and advanced-nursing practice, which applies science and technology to improve healthcare delivery.
Depending on specialty and type of practice, nurse responsibilities are wide-ranging. Here are examples of nurse specialties:
- Ambulatory care nurse. Ambulatory care nurses provide routine medical care for acute illness, chronic disease, and injuries for non-hospitalized or recently discharged patients in outpatient settings.
- Cardiac care nurse. Cardiac care nurses regularly collaborate with cardiologists to treat and care for patients with heart disease and related conditions, including coronary artery disease and congestive heart failure, as well as individuals recovering from bypass surgery.
- Certified nurse-midwife. The CNM’s roots in the U.S. began in 1925. Since then, the role has evolved significantly to provide wide-ranging healthcare services for women and newborns, including prescribing medications in some states.
- Emergency nurse. Emergency nurses work in fast-paced settings — emergency departments, ambulances, and urgent care centers, for example — treating patients with a wide range of illnesses, from injury and fever to respiratory trauma.
- Family nurse. FNPs typically focus on preventive care and the long-term health of individuals of any age, from newborns and children to pregnant and postpartum women and older adults.
Evolution of Nursing Practice
Providing nurses with an evidence-based framework to maximize health outcomes is an important aspect of the evolution of nursing and can be traced back to Nightingale. She documented how deplorable hospital conditions affected soldiers recovering from disease and battle wounds and how hot water and soap helped improve patient care.
Evidence-based practice began appearing in literature in the mid-1990s, but the nursing community didn’t embrace it until the 2000s. In nursing, it’s a systematic approach that integrates clinical expertise with scientific knowledge to improve practice and patient outcomes. For example, a primary tenet in evidence-based practice implementation in nursing includes meeting a patient’s needs and weighing each patient’s experiences and preferences.
Evidence-based practice can also help guide nurses to:
- Identify clinical problems and apply effective interventions correctly
- Evaluate current methods to identify areas for improvement
- Apply new knowledge in clinical practice to further advance nursing science
- Deliver higher quality and safer care to improve patient outcomes
- Make better patient care decisions and eliminate activities of little to no benefit to patients
- Streamline healthcare processes through technology and best practices, saving nurses valuable time
- Provide individualized care to patients
Resources on Nursing Changes Over Time
Learn more about the evolution of nursing practice and the different nurse specialties available today in the following resources:
- Explore Specialties, DailyNurse: This resource provides a list of 200 different nursing specialties.
- “25 Types of Nurses,” Healthline: This resource explores the crucial roles for dozens of nurse specialties.
- Incredible Health, A Complete List of Nursing Types: This guide lists the different types of nurse specialties, with information about degree requirements, responsibilities, and more.
- How To Find Your Nursing Specialty, Nomad: This advice guide breaks down 20 nurse specialty options.
New Developments in Nursing
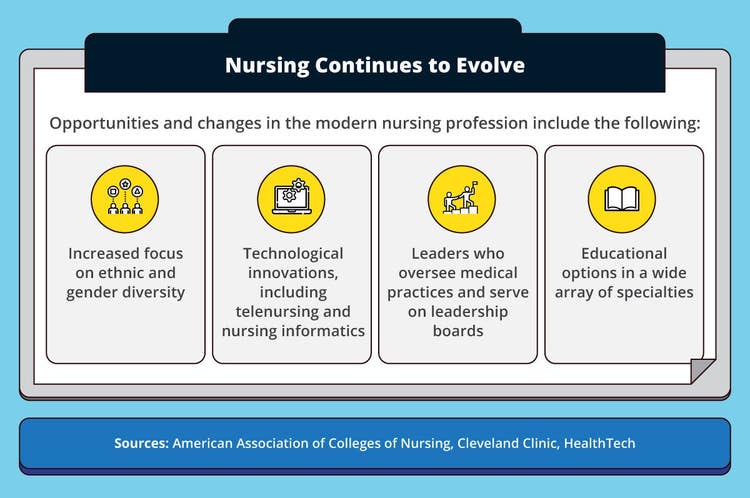
Nursing has grown in complexity since its inception. New developments in nursing, such as the increased use of technology (telehealth, automated equipment, EHRs), have become essential components in care delivery. Additionally, a more diverse nursing workforce helps elevate cultural awareness and empowers nurses to better provide care to people with varied backgrounds.
As the aging population continues to expand and amid the sudden shifts in healthcare that COVID-19 has caused, patient care will become more complex. These developments create opportunities to address these challenges. Here’s a list of major developments in nursing:
- Education. Ever since the first nursing school was established in London in 1860, nursing education has paved the way to modern nursing. Nurses are expected to adapt, and education plays a pivotal role in developing new nurses and preparing them for success. A bachelor’s degree provides nurses with the knowledge to meet the needs of today’s patients and ever-evolving and shifting healthcare environments. Modern nursing education also allows nursing graduates to pursue advanced education and choose from a wide array of careers and specializations.
- Diversity, including ethnicity and gender. Patient populations are more diverse than ever. At the same time, social inequalities that discrimination and other structural factors have created have put some minority groups at risk of not receiving the care they need. The diversification of the nursing workforce helps to address these issues and keep cultural competence at the forefront of patient care.
- Technology, including telenursing and nursing informatics. Data is critical to every aspect of modern society, and it’s no different in the nursing field. Through nursing informatics, healthcare organizations can acquire, process, and assess patient data from different sources, providing enhanced knowledge that can benefit nurses in delivering patient care. Telenursing enables nurses to connect with patients through mobile devices and apps, laptops, videoconferencing technology, and remote patient monitoring.
- Leadership. Nurses such as NPs can now lead medical practice, prescribe medicines, and serve on leadership boards at hospitals.
Resources on Developments in Nursing
For a glimpse of new developments in the evolution of nursing and how they may impact the future of healthcare, the following resources offer some insights:
- Top 16 Nursing Trends That Will Shape Healthcare in 2022, Altus: This resource provides a top 16 countdown of nursing trends in 2022 and beyond.
- “The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity, National Academy of Medicine: This resource includes links to articles, reports, podcasts, and more discussing the future of nursing.
- “What Is Telehealth Nursing: Grow Your Skills,” Relias: This resource examines how telehealth in nursing has been around for many years, and why it’s becoming more prominent today.
Future of Nursing
The U.S. Bureau of Labor Statistics (BLS) reports that 3,080,100 individuals were employed as registered nurses (RNs) in 2020. In terms of job outlook, the future of nursing careers looks promising. The field is expected to grow by 9% from 2020 to 2030, adding about 276,800 new positions, according to the BLS. Due to this growth and other factors such as nurse retirements and career changes, the BLS projects 194,500 RN job openings per year over the period.
The International Council of Nurses reports that there will be a need for up to 13 million more nurses worldwide by 2030. Burnout, retirement, and other factors create challenges in retaining nurses. However, this is also creating job opportunities for new nurses and NPs to help fill the nursing gap.
Additionally, a growing demand exists for nurses with bachelor’s or higher degrees to fill high-level leadership roles. These levels of education provide the clinical preparation and knowledge for nurses to help address challenges in the healthcare industry, including helping alleviate the need and fill the gap of primary care physicians.
In fact, many patients go to FNPs as their primary healthcare providers. In some states, FNPs can even start their own practices. As the need for primary care providers grows, there will be an increased need for nurse leaders who can deliver care and leadership.
Evolve in Your Nursing Career
The work of nurses is critical for the evolution of healthcare systems as many take on increasing responsibility while staying true to their primary purpose: providing high-quality care.
From providing acute care in hospitals to promoting the health of individuals, families, and communities through education, advice, and counseling, the evolution of nursing in modern society has helped advance the U.S. healthcare system and improve the lives of millions of people.
Nursing in modern society also benefits the employment sector. According to a fact sheet from the American Association of Colleges of Nursing (AACN), the nursing profession is the largest in the U.S. healthcare industry, with continued growth and leadership opportunities in the field.
A graduate education is recommended for individuals who want to expand their clinical practice skills and pursue their leadership and goals — for example, becoming NPs. NPs can prescribe medicines, which only medical doctors could do in the past, and launch a primary care practice, thanks to the clinical and leadership knowledge they acquire from an advanced nursing education.
Infographic Sources
American Association of Colleges of Nursing, AACN’s Vision for Academic Nursing
American Association of Colleges of Nursing, Nursing Fact Sheet
Cleveland Clinic, “The Evolution of Nurses as Leaders of Patient Care”
Gallup, “U.S. Ethics Ratings Rise for Medical Workers and Teachers”
HealthTech, “The Impact of Technology in Nursing: Easing Day-to-Day Duties”
Pulse Uniform, 25 Famous Nurses Past to Present World’s Popular Nurse Professionals
Trusted Health, “Black History Month – Notable Nurses Throughout History”
U.S. Bureau of Labor Statistics, Registered Nurses
World Health Organization, Year of the Nurse and the Midwife 2020