Future of Technology in Nursing: How Tech Will Continue Improving Patient Care
Nurses help to administer life-saving medical care to patients across the country and the world on a daily basis. They also interact and communicate with patients to help ensure they feel comfortable and at ease during their health treatment. As such, medical expertise and a good bedside manner are crucial to a nurse’s success in this field.
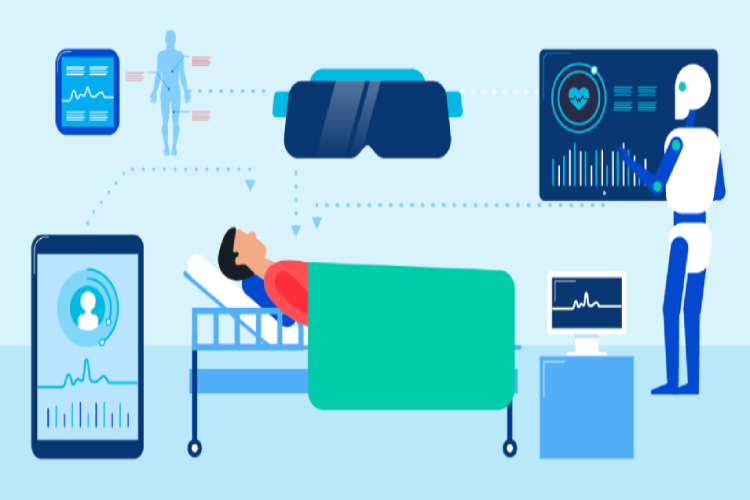
Technology in nursing is also helping to drive medical professionals’ success. Advanced digital tools and devices facilitate a nurse’s job and help ensure that patients receive the best medical treatment possible. As technology has evolved throughout the decades, so has its application and importance in nursing. Nurses use and encourage various types of tech for treating patients, cataloging patient information, and maintaining positive health outcomes even after patients leave a healthcare facility.
Dive into how different types of nursing technology are revolutionizing healthcare.
Electronic Health Records
History of Electronic Health Records
EHRs were first introduced to the healthcare field in the latter half of the 20th century alongside the development and evolution of computer technology. As an article published by the American Health Information Management Association describes, prior to 1992, some organizations used EHRs to assist with billing and scheduling, while others used them for medical care and research purposes.
One fundamental piece of legislation helped pave the way for EHRs to become a commonly accepted piece of medical and nursing technology: 1996’s Health Insurance Portability and Accountability Act, or HIPAA. According to a textbook chapter available from Pearson, “[HIPAA] did not define an EHR, but perhaps the HIPAA Security Rule broadened the definition. The Security Rule established protection for all personally identifiable health information stored in electronic format. Thus, everything about a patient stored in a healthcare provider’s system is protected and treated as part of the patient’s EHR.”

Benefits of Electronic Health Records
A Holistic Portrait of a Person’s Health History
If a patient visits a hospital with complaints of back pain, an attending physician may ask about their symptoms, evaluate their current physical condition, review the information in their health records, and make a diagnosis based on their findings.
However, if those health records contain incomplete or faulty information, the physician may make a misdiagnosis or not understand what is causing the patient’s back pain. An EHR that contains extensive data about a patient’s health history can include comments from previous physicians, past treatments or surgeries, medications currently and previously taken, notes about family health history, and other important information.
Fewer Errors and Less Red Tape
Numerous errors can result from a physician, nurse, patient, or other health professional using a health record that is not in an electronic format. A paper record may be easily damaged or lost in a conventional filing system, a record from one facility may not be fully interpreted or accessed by officials at another facility, and patients and professionals may input or misunderstand the information present in the records. EHRs help to alleviate these issues by offering a secure, convenient, and comprehensive method for storing a patient’s health info.
Additionally, EHRs can reduce the lengthy processes and red tape often associated with collecting and transferring healthcare records. With a paper record system, officials at one facility may have to wait an extended period of time for a patient’s records to arrive before treating that individual. With an EHR, that type of transfer can occur much faster. A patient who is curious to learn more about their health history can also access their EHR immediately rather than having to wait to hear back from a clinic or physician.
Mobile Functionalities
Challenges of Electronic Health Records
Different EHR Systems
A patient may visit a health clinic in their neighborhood and learn that they need to consult with a specialist at a state hospital many miles away. The state hospital staff may use an EHR system that is different from the smaller health clinic’s system, making it more difficult to transfer records efficiently.
The fact that there is not one fully integrated system or platform used by all health clinics and organizations can create more issues regarding red tape, even though EHRs are partly intended to help reduce such health and nursing technology issues. It can also mean that information isn’t properly transferred or collected and that staff and health officials are not fully trained on how to use multiple EHR systems.
Security and Privacy Concerns
EHRs are stored and secured digitally. While this has allowed for more convenient access and use by healthcare officials, the records and the confidential information they contain can be infiltrated, damaged, and exposed by individuals with nefarious intent.
Data breaches by hackers and digital criminals can expose confidential health information — such as a person’s medical history, address, or payment info — to a wide audience. Additionally, the fact that an EHR can be so widely accessible from multiple points raises concerns regarding patient privacy, even if the information is kept secure.
Future of Electronic Health Records
In an article published in HealthcareItNews, Carl Dvorak, president of healthcare software company Epic Systems, points to factors such as telemedicine and advanced analytics as future areas that will impact the development and evolution of electronic health records.
Genomics – the study of human genes and their functions – will also allow for a larger and more precise collection of specialized information about a patient’s health history. And telehealth, the burgeoning nursing and health technology field in which healthcare is administered and delivered remotely, can help to broaden the scope of EHRs and their efficient use in healthcare environments.
Robotics and Artificial Intelligence
History of Robotics and AI in Nursing
Types and Current Use of Robotics and AI in Nursing
Robotics have been employed across many areas of nursing and healthcare. In some clinics, “friendly” hospital robots have helped to assist stressed nurses. In surgical situations, robotic surgical and nursing technologies, such as the da Vinci Surgical System, have led to better patient outcomes.
Plus, AI is helping healthcare professionals to better sort through patient data and improve the accuracy of diagnoses. For example, AI can help analyze large data sets and determine if a particular condition is a result of a person’s own health or may be due to larger factors, such as a high number of recent outbreaks of disease in a given community or trends of poor dietary habits in certain populations.

Benefits of Robotics and AI in Nursing
A Range of Healthcare Services
Reduced Labor Costs
Enhanced Training
Improved Patient Outcomes
Challenges of Robotics and AI in Nursing
Privacy Issues and Concerns
A patient who visits a health clinic, fills out an insurance form, or seeks to have a prescription refilled is providing health data. However, that patient may not know that AI tools are being used to evaluate that data as part of a larger collection or to better predict and reach health outcomes.
This lack of privacy can present challenges to patients who wish to better safeguard their personal health information. As healthcare environments become more reliant on technology, this issue will only become more difficult to address in the future.
Lack of Empathy When Treating Patients
Ethical and Legal Issues
Future of Robotics and AI in Nursing
According to an article from RN.com, “Despite these advancements, questions remain about whether the pricey new technology can actually deliver reliable and consistent results [in clinical settings]. Only time will tell … but in the meantime, nurses can prepare themselves for more innovative changes in the way care is delivered by embracing these new technologies.”
In short, advances in technology always spark a combination of advantages and challenges in healthcare. Ultimately, though, the benefits that robotics/AI bring as nursing technologies outweigh the drawbacks.
Robotics and AI in Nursing: Resources
Robotic and AI systems are now being utilized in hospitals around the world. Here are a few examples:
- The DaVinci Surgical System was one of the first robotic surgical assistant systems. Launched in 1999, it’s not an autonomous robot; rather, it allows doctors to perform procedures with instruments that the doctor operates via a control panel.
- In Japan, the use of robot nurses has increased, in large part due to that country’s nursing shortage. Robear, a robot developed by the Riken corporation, is used to lift and move elderly and immobile patients.
- Mabu is a medical robot developed by Catalia Health. Launched in 2018, the 15-inch tall robot engages patients in conversation, and asks them for updates on their health, activity, and whether or not they’ve taken any prescribed medications.
- Aethon’s TUG autonomous robot assists nurses and doctors by literally doing the heavy lifting; this robot was designed to move medical supplies and equipment around hospitals, freeing up medical staff to focus on caring for patients.
Deploying a robotics system in a hospital presents multiple challenges, and hospital administrators should understand the benefits and drawbacks. The National Institutes of Health provides this overview of the state of robotics in hospitals.
Wearable Devices
History of Wearable Devices
Types and Current Use of Wearable Devices
Benefits of Wearable Devices
A Remote Snapshot of a Person’s Health
Improved Patient Outcomes and Fewer Primary Care Visits
Monitoring Patients from Afar
Challenges of Wearable Devices
Issues with Price and Technology
Privacy Concerns
Accuracy/Misinterpretation Concerns
Future of Wearable Devices
Wearable devices have been projected to advance as far as, for example, Google Glass goggles providing a better understanding of how to perform surgery or helping children with autism to better communicate in class. Wearables are also being tested on athletes to measure electrolyte loss, among other things, and are continuing to help improve heart disease and other conditions.
Despite the challenges that this technology may face, the potential for wearables is vast. Professionals who understand the technology’s full scope and its applications will be best suited for helping patients.