How Nurses Impact Quality of Care
Imagine an elderly patient undergoing home healthcare who has no nearby family and who struggles with mobility, making it difficult to leave the house. A nurse providing care in this situation needs to be technically skilled and able to effectively administer medication and monitor medical conditions, but beyond these standards of care, a nurse can have a deeper impact. Companionship, compassion, and other skills outside of the technical realm can all improve a patient’s quality of life.
Nurses are critical to patient health, patient satisfaction, and the overall quality of care that individuals receive. Because of their direct contact with patients, nurses are uniquely positioned to build relationships and advocate for patients in settings such as hospitals, doctors’ offices, and nursing homes.
As for offering the highest quality of care, nurses need to be aware of many factors, such as effective communication and patient empathy, and take a person-centered approach to all that they do. These elements combine to create effective care and better health outcomes. Nurses need to strive to be lifelong learners throughout their careers.
The nursing field is expansive and requires that nurses juggle a multitude of hard and soft skills, all of which can impact the overall quality of care. These skills include communication and empathy, as well as field-specific skills learned during formal nursing education.
Skills and Characteristics of High-Quality Nurses
High-performing nurses use many emotional, social, and technical skills every day. Among the most vital skills for nurses are:
- Communication: Communication skills are key to good nursing. As part of a team, a nurse needs to listen to and follow directions from doctors and communicate with patients and their families. Communication skills also include patient advocacy; as some patients may not have the knowledge or confidence to speak up for themselves in a hospital setting, nurses must translate “medical speak,” or medical jargon; discuss health issues and solutions; and help patients articulate questions regarding their health and well-being.
- Respect: To truly provide a high quality of care, nurses should never become desensitized to their patients’ humanity and must always exercise a high degree of respect. Successful nurses maintain a professional demeanor, take confidentiality seriously, and keep patients’ wishes at the forefront of treatment.
- Organization: Since nurses are often the people administering medication and maintaining patient records, organizational skills can be a matter of life and death. Even in hectic environments, nurses need to pay close attention to detail and monitor and document changes in a patient’s health or medications.
- Empathy: Empathy in nursing can be challenging because nurses must simultaneously maintain professional boundaries, yet it remains vital to quality nursing care. Empathic nurses make patients feel seen and heard as individuals.
- Lifelong learning: Healthcare changes quickly, particularly in terms of technology. Nurses need to continue to learn and grow throughout their careers, whether through continuing education, professional conferences, or on-site professional development.
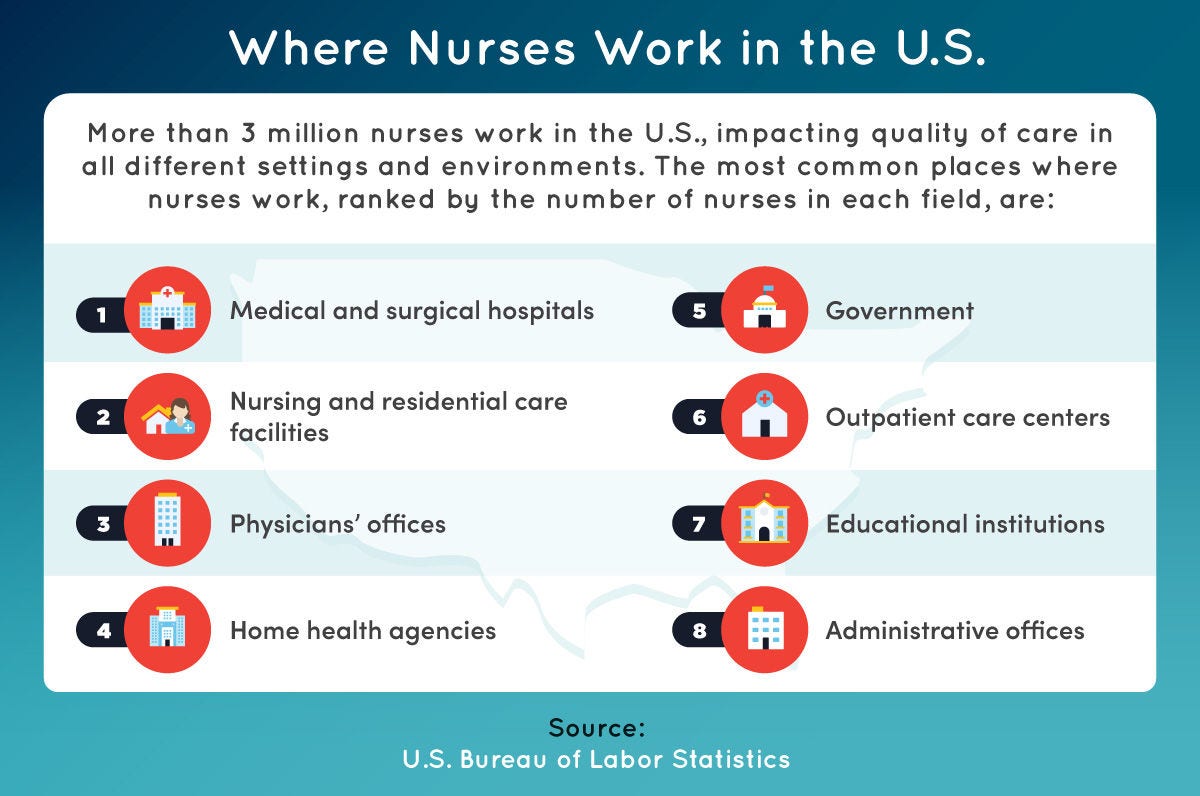
More than 3 million nurses work in the U.S., impacting quality of care in all different settings and environments. The most common places where nurses work, ranked by the number of nurses in each field, are medical and surgical hospitals; nursing and residential care facilities; physicians’ offices; home health agencies; government; outpatient care centers; educational institutions; and administrative offices.
Impact of Nurses in Healthcare Settings
Nurses impact quality of care in various healthcare settings, including the following:
- Doctors’ offices: In doctors’ offices, nurses are the providers who see patients before the doctors, so their presence can set the tone for an entire visit.
- Hospitals: Hospital visits can be extremely stressful for patients, and nurses can serve as a calming presence during an anxiety-inducing experience.
- Nursing homes: In nursing homes or other long-term care facilities, nurses often serve as companions and medical professionals.
- Home care: Home care is an opportunity for relationship building between nurses and their patients.
- Hospice: In end-of-life care, or hospice care, nurses serve an important role for both patients and their families, making patients comfortable and helping ease the transition.
- Community care settings: Nurses often work in community care settings, such as rehab facilities or homes for adults with disabilities. In these settings, nurses have a chance to build long-term relationships with patients and their families.
Patient satisfaction measures how well a patient’s expectations are met. Patient satisfaction is central for many reasons, not only because satisfaction often correlates with improved patient outcomes, but also because patient satisfaction is linked to measures such as federal funding for hospitals and healthcare agents.
Patient satisfaction is usually assessed through follow-up surveys or phone calls. Health institutions analyze the data from these surveys and use it to create action plans to improve the institution as a whole. In 2002, the first such survey on patient perspectives, the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS), was administered to hospital patients after discharge to assess their satisfaction in various critical areas. According to the Centers for Medicare and Medicaid Services, the areas are “communication with nurses and doctors, the responsiveness of hospital staff, the cleanliness and quietness of the hospital environment, communication about medicines, discharge information, overall rating of hospital, and would they recommend the hospital.”
Nurses figure prominently in these assessments because they directly interact with patients every day. In many cases, a nurse is the healthcare point person who spends the most time with a patient and most directly drives patient satisfaction. Aspects of patient satisfaction that nurses directly affect include the amount of time providers spend with a patient, the clarity of the information provided, and the accessibility of tools and strategies to improve health.
Patient satisfaction can often be improved by ensuring that a facility has adequate nurse staffing to effectively communicate with patients. Increasing the amount of time that nurses can spend with each patient (another byproduct of employing a sufficient number of nurses) is another way that patients feel well taken care of. Patient satisfaction can also be improved by training doctors and nurses in effective communication strategies so all patients walk away with a better understanding of their health and treatment options.
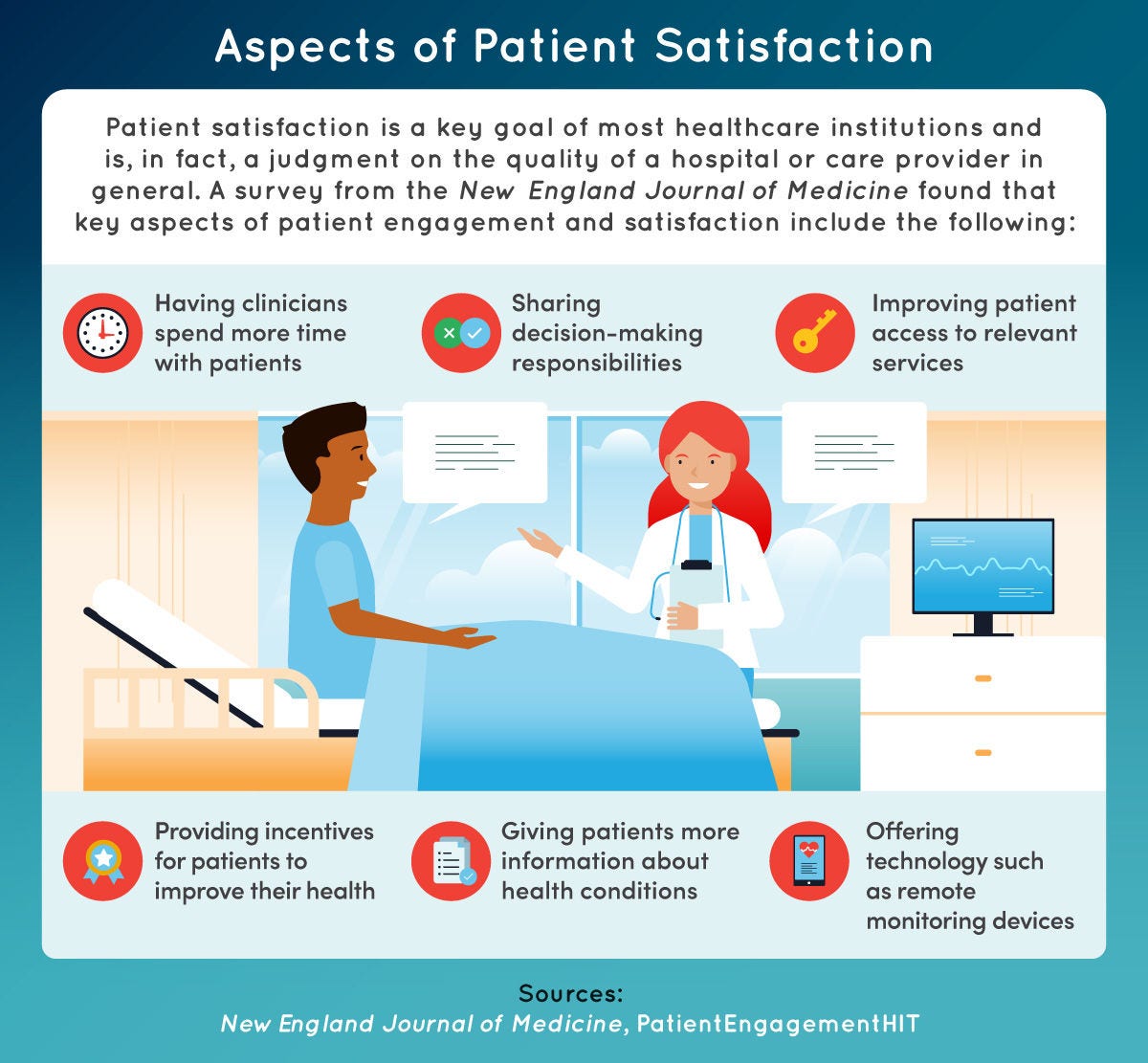
Patient satisfaction is a key goal of most healthcare institutions and is, in fact, a way to evaluate the quality of a hospital or care provider in general. A survey from the New England Journal of Medicine found that key aspects of patient engagement and satisfaction include the following: having clinicians spend more time with patients; sharing decision-making responsibilities; improving patient access to relevant services; providing incentives for patients to improve their health; giving patients more information about health conditions; and offering technology such as remote monitoring devices.
Nurses are of utmost importance in the chain of communication in any healthcare setting. The proper functioning of this communication chain directly impacts patient safety in various ways. Sometimes, healthcare providers make assumptions about what patients and their families know about health-specific vocabulary, such as anatomy and medication. A skilled nurse knows how to check for understanding and clearly explain important details in easy-to-understand language.
In some cases, especially in short-staffed facilities, nurses may not have enough time for questions after explaining a patient’s diagnosis or medication regimen. This can have grave consequences, even endangering a patient’s life. As the liaison between doctors and patients, nurses are a vital link between communication and patient safety, ensuring that patients truly understand the most important elements of their health.
Types of Communication
All the different types of communication can be put to work in a healthcare setting to maximize the quality of care. However, four key types of communication are important for nurses to understand and employ.
- Verbal communication: Verbal communication commonly refers to what a person says. Clear verbal communication includes the use of a strong speaking voice with appropriate volume and speed as well as the elimination of filler words, such as “um” and “like.” Verbal communication also includes active listening skills to ensure that others understand. Nurses need to have strong verbal communication skills so patients can not only hear what they’re saying but also understand.
- Nonverbal communication: Nonverbal communication includes gestures, body language, and facial expressions. Nurses can exhibit strong nonverbal communication by making strong eye contact; offering positive body language, such as good posture and a welcome, opening stance; and smiling when greeting a patient to develop rapport.
- Written communication: In written communication with patients or doctors, nurses should focus on simplicity. In communicating with patients and families, nurses should avoid medical jargon or terms that may be confusing, instead opting for concise, clear sentence structures. Other important aspects of written communication include attention to tone and thorough editing before sharing with others.
- Cultural awareness: Knowledge of cultural norms that may be outside of a nurse’s own culture is key to effective communication. For example, in many cultures, direct eye contact is seen as a sign of disrespect. If nurses understand this and other norms, they’ll recognize that a patient may be avoiding eye contact to show respect — not because of anxiety or embarrassment — and they’ll be better able to convey their own respect for the patient.
Patient empathy involves understanding and sharing a patient’s feelings. Empathy is a strong predictor of patient satisfaction and figures prominently into quality of care.
Empathy includes three primary branches: affective, cognitive, and behavioral. In nursing, affective empathy means that a nurse recognizes patients as individuals rather than indistinct “customers.” Cognitive empathy refers to interpersonal sensitivity and encompasses verbal and nonverbal communication that allows a nurse to get to know a patient on a deep level and create a space of comfort and kindness. Behavioral empathy refers to a nurse using a high degree of sensitivity to actively advocate for a patient to help relieve pain and improve health.
Nurses practice patient empathy every day by listening to patients, communicating verbally and nonverbally, and establishing a high level of advocacy and care. Maintaining patient empathy can lead to a syndrome called “compassion fatigue”: physical and psychological exhaustion that helping professionals and caregivers often experience.
Compassion fatigue can result in withdrawal, shifts in mood, and irritability. For nurses, who need to exercise a high degree of compassion on the job every day, it can be a serious condition. Taking time off, investing time in hobbies, and talking through stress and traumatic events with a trusted friend or professional counselor can help prevent burnout.
Empathy doesn’t come naturally to all nurses, but they can develop it like any other skill. Studies have shown that about 70% of healthcare workers find it difficult to empathize with patients. Some ways to improve empathy on the job include practicing emotional regulation skills through mindfulness or meditation as well as finding a strong support system among co-workers. Healthcare facilities can reduce burnout in nurses and improve empathy by limiting the number of patients nurses see in a day and creating a positive workplace environment with reasonable hours and appropriate breaks.
Patient empathy has tremendous benefits, creating a more positive patient experience. Patients who interact with empathic nurses are more likely to follow recommendations for at-home care. Studies have shown that cancer patients who experience patient empathy also exhibit less stress and depression during treatment, and expectant mothers experience less fear and anxiety prior to labor.
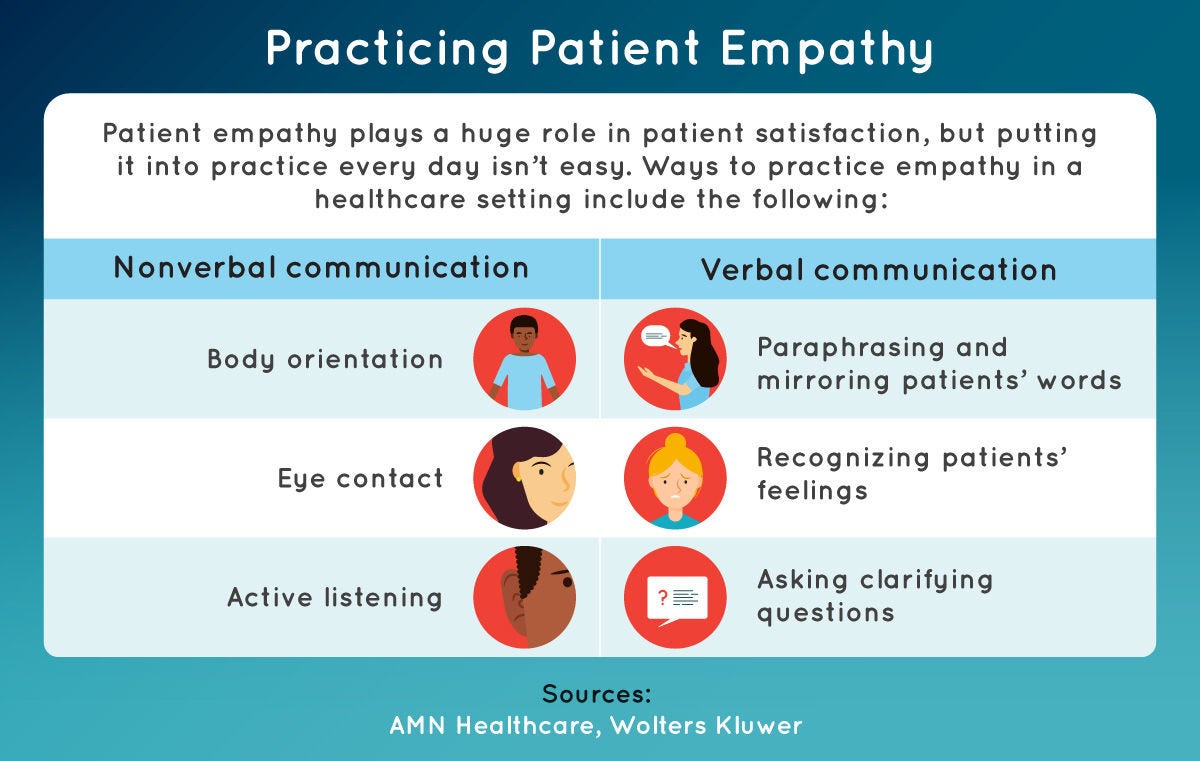
Patient empathy plays a huge role in patient satisfaction, but putting it into practice every day isn’t easy. Ways to practice empathy in a healthcare setting include nonverbal communication, such as body orientation, eye contact, and active listening; and verbal communication, such as paraphrasing and mirroring patients’ words, recognizing patients’ feelings, and asking clarifying questions.
Person-centered healthcare is an approach that views patients as equal partners in planning, developing, and monitoring care to meet their needs. In contrast to a task-centered approach that views patients as commodities or projects, person-centered care focuses on relationship building, patient empathy, and the core understanding that each patient is a human being with unique needs and wants.
Although not yet the norm, person-centered healthcare is becoming more widely practiced and has been linked to improved health outcomes. Person-centered healthcare requires a shift in thinking, approach, and service delivery. Often, large healthcare institutions take a task-centered approach because of the sheer volume of patients entering their facilities each day. On a systemic level, institutions can begin to adopt a person-centered approach by reducing the number of patients that each provider sees.
Core Aspects of the Person-Centered Approach
The person-centered approach to healthcare includes several core aspects:
- Respect and value: A person-centered approach values and respects patients as full members of society. Regardless of factors such as age, language, or socioeconomic status, nurses using a person-centered approach value patients and involve them as partners in their care.
- Individualized care: Rather than simply treating a diagnosis, nurses taking a person-centered approach will provide individualized physical and emotional care spaces that align with their patients’ changing needs.
- Understanding: The person-centered approach requires that providers understand patients’ perspectives in care and activities.
- Opportunities for engagement: Nurses using a person-centered approach work to provide opportunities for social engagement to encourage patient well-being.
A person-centered approach can lead to higher patient satisfaction and better health outcomes because it creates a sense of mutual respect and collaboration. Person-centered care can play out in many ways; for example, a patient in a long-term care facility who’s offered opportunities for social engagement may experience reduced loneliness, stress, or depression. A patient receiving cancer care may find comfort in a nurse who practices great communication and patient empathy. Patients with diabetes who encounter a nurse using person-centered tenets have been shown to more effectively manage their condition and experience overall improved health outcomes.
Additional Resources: Person-Centered Care
Nurses can explore various resources that examine person-centered care.
- UB Institute for Person-Centered Care: Created to administer better health delivery systems to the vulnerable, the UB Institute for Person-Centered Care provides a wealth of information on advocacy, awareness of patient needs, research, and practical professional development.
- Pioneer Network: Long-term care and care for the aging benefit greatly from a person-centered approach. Pioneer Network provides resources for person-centered and patient-directed care for the aging.
- Health Leads, Patient-Centered Care: Elements, Benefits, and Examples: A basic primer on patient-centered care, how it’s practiced, and its benefits.
- American Journal of Managed Care, “Contributor: A Vision for Patient-Centered Core Impact Sets: A Unifying Approach to Patient Centricity”: An article on providing high-value healthcare in an overburdened system and how treatment impacts the lives of patients.
- The Hill, “Telehealth May Finally Shift Healthcare to Be Patient-Centered”: A brief discussion of the impact of telehealth on quality of care.
Achieving Satisfaction via Quality of Care
Nurses impact quality of care in various ways. They use both hard and soft skills to provide quality of care in settings such as hospitals, nursing homes, and community care settings. Nurses affect patient satisfaction throughout daily operations by their direct interaction with patients. Nurses use interpersonal skills to ensure smooth communication and patient safety and practice patient empathy and person-centered care to supply patients with unique care that meets their individual needs and expectations.
These elements of nursing care not only make for a better patient experience but also lead to better health outcomes. Since nurses are the providers who interact with patients most directly, they help patients better understand their own health needs and increase the likelihood that they’ll follow medical recommendations. Increased education and training in person-centered care can help nurses be even more effective in their work, increasing patient satisfaction and improving outcomes.

